The Ultimate 5Step Guide To Designing Your Pa Program Today
Introduction to Designing Your PA Program

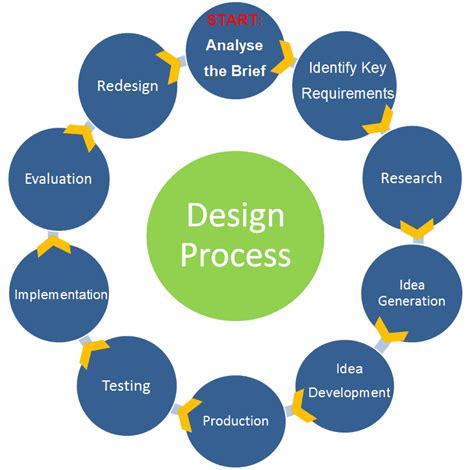
Designing a successful Physician Assistant (PA) program requires careful planning and consideration of various factors. In this comprehensive guide, we will walk you through the essential steps to create an effective and engaging PA curriculum. Whether you are a medical educator, program director, or an aspiring PA student, this step-by-step approach will help you navigate the process and develop a robust program.
Step 1: Define the Program’s Vision and Goals
Before diving into the curriculum design, it is crucial to establish a clear vision and set specific goals for your PA program. This step lays the foundation for the entire curriculum development process.
Vision Statement
Craft a concise and inspiring vision statement that reflects the program’s philosophy and values. Consider the following questions:
- What is the primary purpose of your PA program?
- How do you envision the role of PAs in the healthcare system?
- What unique attributes or specialties do you want to emphasize?
For example, your vision statement could be: “Our PA program aims to educate and train highly competent, compassionate, and culturally sensitive healthcare professionals who will contribute to the diverse needs of our community.”
Program Goals
Define measurable and achievable goals that align with your vision. These goals should address the knowledge, skills, and attitudes you want your PA graduates to possess. Some common goals include:
- Providing a comprehensive and evidence-based curriculum that covers all essential areas of medical practice.
- Developing critical thinking and problem-solving skills in PA students.
- Promoting cultural competence and sensitivity in patient care.
- Ensuring clinical proficiency through hands-on training and supervised practice.
- Preparing PA graduates for successful licensure and certification examinations.
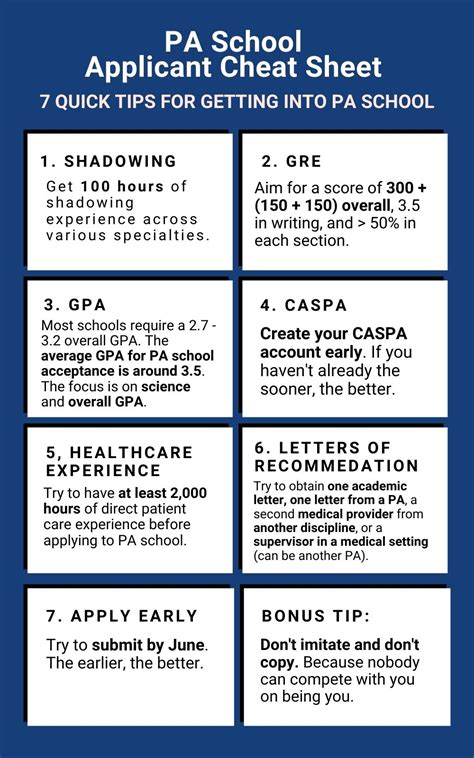
Step 2: Conduct a Comprehensive Needs Assessment

A needs assessment is a crucial step to understand the requirements and challenges specific to your program and target audience. It helps identify gaps and areas for improvement.
Gather Data
Collect data from various sources to gain a comprehensive understanding of the healthcare landscape and the needs of your community:
- Review existing literature, research studies, and reports related to PA education and healthcare trends.
- Conduct surveys and interviews with healthcare professionals, including physicians, nurses, and current PAs, to gather their insights and experiences.
- Analyze data on healthcare service utilization, disease prevalence, and demographic trends in your region.
- Engage with key stakeholders, such as healthcare facilities, hospitals, and community organizations, to understand their needs and expectations from PA graduates.
Identify Gaps and Priorities
Analyze the collected data to identify gaps in healthcare services, emerging healthcare needs, and areas where PAs can make a significant impact. Prioritize these needs based on their relevance and urgency. Some examples of identified gaps could include:
- Lack of access to primary care services in rural areas.
- Rising demand for specialized PA services, such as geriatric care or mental health support.
- Need for culturally competent healthcare providers to serve diverse populations.
- Gaps in healthcare infrastructure, such as limited access to diagnostic tools or specialized equipment.
Step 3: Develop the Curriculum Framework

With a clear vision, defined goals, and a thorough needs assessment, you are now ready to develop the curriculum framework. This step involves structuring the curriculum to align with your program’s objectives and address the identified needs.
Curriculum Components
Your curriculum should consist of several key components, including:
- Basic Sciences: Covering essential medical sciences such as anatomy, physiology, pharmacology, and pathology.
- Clinical Skills: Developing practical skills in physical examination, diagnostic procedures, and clinical decision-making.
- Clinical Medicine: Providing in-depth knowledge of various medical specialties, including internal medicine, surgery, pediatrics, and emergency medicine.
- Public Health and Preventive Medicine: Focusing on population health, health promotion, and disease prevention.
- Professionalism and Ethics: Emphasizing the importance of ethical conduct, patient-centered care, and professional development.
- Interprofessional Collaboration: Promoting teamwork and effective communication with other healthcare professionals.
Curriculum Mapping
Create a curriculum map that outlines the sequence and integration of courses and clinical experiences. Consider the following:
- Course Sequence: Determine the order in which courses should be taken, ensuring a logical progression of knowledge and skills.
- Clinical Rotations: Design clinical rotations that provide a diverse range of experiences, allowing students to apply their knowledge in real-world settings.
- Elective Options: Offer elective courses or rotations to allow students to explore their areas of interest or specialize in specific fields.
- Continuity Clinics: Implement continuity clinics where students can establish long-term relationships with patients and gain experience in ongoing care.
Step 4: Implement and Evaluate the Curriculum
Once the curriculum framework is developed, it’s time to implement and continuously evaluate its effectiveness. This step ensures that the curriculum remains relevant, engaging, and aligned with the program’s goals.
Implementation Strategies
- Faculty Development: Provide training and support to faculty members to ensure they are equipped with the necessary skills and resources to deliver the curriculum effectively.
- Resource Allocation: Allocate adequate resources, including facilities, equipment, and teaching materials, to support the curriculum implementation.
- Student Support Services: Offer academic advising, tutoring, and mentorship programs to assist students in their learning journey.
- Clinical Site Partnerships: Establish strong partnerships with clinical sites to ensure a diverse range of high-quality clinical experiences for students.
Continuous Evaluation and Improvement
- Curriculum Review: Regularly review and update the curriculum to incorporate new advancements in medical knowledge and practice.
- Student Assessment: Implement a comprehensive assessment system to evaluate student learning outcomes and provide feedback for improvement.
- Alumni and Employer Feedback: Collect feedback from program alumni and employers to understand the program’s impact and identify areas for enhancement.
- Research and Scholarship: Encourage faculty and students to engage in research and scholarly activities to contribute to the advancement of PA education and practice.
Step 5: Foster a Culture of Continuous Improvement

Designing a PA program is an ongoing process, and it is essential to create a culture that values continuous improvement and innovation.
Professional Development
- Faculty Professional Development: Encourage faculty members to engage in ongoing professional development, such as attending conferences, workshops, and online courses, to stay updated with the latest advancements in PA education.
- Student Leadership and Engagement: Provide opportunities for students to take on leadership roles, participate in student organizations, and contribute to program improvement initiatives.
Adaptability and Flexibility
- Curriculum Flexibility: Be open to adapting the curriculum based on emerging healthcare needs, changes in medical practice, and student feedback.
- Innovation in Teaching Methods: Explore innovative teaching strategies, such as simulation-based learning, interprofessional education, and online learning, to enhance student engagement and learning outcomes.
Conclusion

Designing a PA program requires a thoughtful and comprehensive approach, considering the unique needs of your community and the evolving healthcare landscape. By following these five steps—defining the program’s vision and goals, conducting a needs assessment, developing a curriculum framework, implementing and evaluating the curriculum, and fostering a culture of continuous improvement—you can create a robust and impactful PA program. Remember, the key to success lies in maintaining a student-centered approach, staying adaptable, and continuously seeking feedback and improvement.
FAQ

How long does it take to design a PA program curriculum?
+The timeline for designing a PA program curriculum can vary depending on several factors, including the availability of resources, the complexity of the program, and the involvement of key stakeholders. On average, it can take anywhere from 6 months to 2 years to develop a comprehensive curriculum. However, it is important to note that curriculum design is an ongoing process, and continuous evaluation and improvement are essential to ensure its effectiveness.
What are the key considerations when selecting clinical rotation sites for PA students?
+When selecting clinical rotation sites, it is crucial to consider factors such as the diversity of patient populations, the range of medical conditions and specialties available, and the quality of supervision and mentorship provided. Additionally, ensuring that the clinical sites align with the program’s vision and goals, and offer opportunities for students to gain practical experience in their areas of interest, is essential.
How can PA programs promote cultural competence and sensitivity among students?
+Promoting cultural competence and sensitivity is vital in PA education. Programs can achieve this by incorporating cultural competency training into the curriculum, encouraging students to participate in community service activities that involve diverse populations, and providing opportunities for students to interact with patients from different cultural backgrounds during clinical rotations. Additionally, incorporating diverse faculty and staff who can serve as role models and mentors can further enhance cultural competence.
What are some best practices for faculty development in PA programs?
+Faculty development is crucial for the success of any PA program. Best practices include providing regular professional development opportunities, such as workshops, conferences, and online courses, to keep faculty members updated with the latest advancements in PA education and medical knowledge. Additionally, encouraging faculty collaboration, mentorship programs, and feedback mechanisms can enhance teaching effectiveness and student learning outcomes.
How can PA programs ensure the curriculum remains relevant and up-to-date?
+To ensure the curriculum’s relevance and currency, PA programs should establish a culture of continuous improvement and innovation. This includes regularly reviewing and updating the curriculum based on feedback from students, alumni, and employers, as well as staying abreast of advancements in medical practice and healthcare trends. Additionally, engaging in research and scholarly activities can contribute to the program’s reputation and enhance its curriculum’s quality.

